| DIABETES
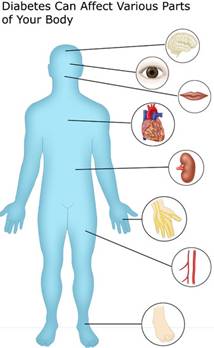
Diabetes mellitus is a metabolic cum vascular disorder in which the body’s capacity to utilize glucose, fat and protein is disturbed due to insulin deficiency and/or insulin resistance. This could lead to damage of blood vessels if left uncontrolled. In people with diabetes there is insufficient insulin activity in the body. Insulin is a hormone produced by beta cells of islets of Langerhans in the pancreas. In diabetics, the body does not produce enough insulin or does not use the produced insulin effectively. This results in a high level of glucose in the blood ("hyperglycemia").
1. TYPES OF DIABETES
2. SYMPTOMS OF DIABETES
3. DIAGNOSIS
4. DIABETIC RETINOPATHY
5. DIABETES AND KIDNEY
6. DIABETES AND FEET
7. PREVENTION OF DIABETES
8. DIET AND DIABETES
Top
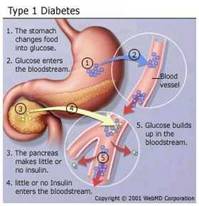
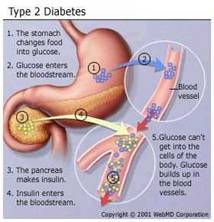
There are four main types of diabetes mellitus
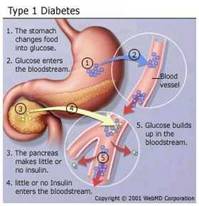
a)Type 1, earlier known as insulin dependent diabetes mellitus (IDDM) or juvenile-onset diabetes mellitus. People with this type of diabetes make little or no insulin in their body, and need regular insulin injections for survival and management of diabetes. It usually starts in childhood, but can occur at any age.
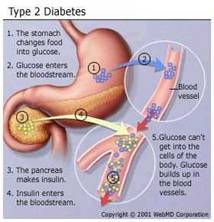
b) Type 2 (DM2), earlier known as non-insulin dependent diabetes mellitus (NIDDM) or adult-onset diabetes. This is the most common form of diabetes, and is strongly associated with genetic tendency and obesity. The body produces normal or even high levels of insulin, but certain factors make its utilization ineffective ("insulin resistance"). Sedentary lifestyle, unhealthy dietary patterns, and the consequent obesity are common causes. It usually starts in adulthood, but is beginning to be seen in obese adolescents also.
c) Gestational diabetes mellitus or pregnancy-induced diabetes. Gestational diabetes is usually identified during the second trimester of pregnancy. In this condition, the pregnancy hormones inhibit the action of insulin due to which the glucose produced in the body is not utilised for providing energy. The glucose level in the body increases leading to hyperglycaemia and the body tissues are deprived of energy. High blood sugar can damage the health of the fetus. Some of the complications for the baby include premature delivery, respiratory problems, congestive heart failure and decreased ability to tolerate labour.
d) Secondary diabetes mellitus, caused by genetic conditions, pancreatic diseases (e.g. inflammation, surgery or malignancy of the pancreas, etc.), drugs (e.g. steroids like prednisolone, pentamidine, excess thyroid hormone, etc.) or other medical conditions (acromegaly, Cushing syndrome, pheochromocytoma, hyperthyroidism, congenital rubella, etc). Medications such as thiazide diuretics or oral contraceptives can precipitate diabetes in a person predisposed to get it later.
Action of insulin on the food
Most of the food we eat is broken down into glucose and other simple sugars. Glucose gets absorbed into the blood stream which enters into the cells and is used for energy. As the blood glucose rises, insulin is released from the pancreas. Cells have receptor sites on the outside. When insulin attaches to the receptor sites, a passage is made and glucose enters into the cell. Thus insulin regulates the blood glucose level. When there is an insulin deficiency, glucose cannot enter into the cells and remains in the blood which leads to high blood sugar levels.
Normal Plasma Glucose Levels:
Fasting 70–100mg/dl
Post Prandial 100–140mg/dl
Insulin deficiency may be relative or absolute and may be due to
1. Insufficient production of insulin by the pancreas.
2. Sufficient production of insulin but non release into the blood stream.
3. Increased demand for insulin by the body tissues.
4. Destruction / Inactivation of insulin by enzymes and other factors produced by the liver and endocrine glands such as pituitary gland, adrenal cortex, thyroid etc.,
RISK FACTORS FOR DIABETES
1. Family history of diabetes.
2. Over weight / Obesity.
3. High blood pressure or hyperlipidemia.
4. Those with previous bad obstetric history.
a. Recurrent abortions b. Still births c. Congenital malformations d. Big baby (over 3.5 kg at birth)
5. Mental stress
6. Physically inactive people (sedentary jobs).
2. SYMPTOMS OF DIABETES
Top
1. Increased thirst.
2. Increased hunger.
3. Excessive urination.
4. Weight loss.
5. Weakness and tiredness.
6. Delayed wound healing.
7. Numbness in hands and feet.
8. Blurred vision.
9. Itching in genitals.
3. DIAGNOSIS
Top
Diabetes mellitus is diagnosed based on a high level of glucose or sugar in the blood. The doctor may suspect diabetes mellitus after taking the medical history and doing a physical examination.
The following tests are used for diagnosis:
-
Fasting plasma glucose test measures blood glucose after the person have gone at least 8 hours without eating. This test is used to detect diabetes or pre-diabetes.
-
An oral glucose tolerance test measures blood glucose after the person have gone at least 8 hours without eating and 2 hours after drinking a glucose-containing beverage. This test can be used to diagnose diabetes or pre-diabetes.
-
In a random plasma glucose test, doctor checks the person blood glucose without regard to when the person ate his/her last meal. This test, along with an assessment of symptoms, is used to diagnose diabetes but not pre-diabetes.
Positive test results should be confirmed by repeating the fasting plasma glucose test or the oral glucose tolerance test on a different day.
Fasting Plasma Glucose (FPG) Test
The FPG is the preferred test for diagnosing diabetes due to convenience and is most reliable when done in the morning. Results and their meaning are shown in table 1. If the fasting glucose level is 100 to 125 mg/dL, the person have a form of pre-diabetes called impaired fasting glucose (IFG), meaning that the person is most likely to develop type 2 diabetes but do not have it yet. A level of 126 mg/dL or above, confirmed by repeating the test on another day, means that you have diabetes.
Table 1. Fasting Plasma Glucose Test
| Plasma Glucose Result (mg/dL) |
Diagnosis |
99 and below |
Normal |
100 to 125 |
Pre-diabetes
(impaired fasting glucose) |
126 and above |
Diabetes* |
*Confirmed by repeating the test on a different day.
Oral Glucose Tolerance Test (OGTT)
Research has shown that the OGTT is more sensitive than the FPG test for diagnosing pre-diabetes, but it is less convenient to administer. The OGTT requires the person to fast for at least 8 hours before the test. That persons plasma glucose is measured immediately before and 2 hours after he/she drink a liquid containing 75 grams of glucose dissolved in water. Results and what they mean are shown in table 2. If the persons blood glucose level is between 140 and 199 mg/dL 2 hours after drinking the liquid, he/she have a form of pre-diabetes called impaired glucose tolerance or IGT, meaning that he/she is more likely to develop type 2 diabetes but do not have it yet. A 2-hour glucose level of 200 mg/dL or above, confirmed by repeating the test on another day, means that the person have diabetes. Table 2. Oral Glucose Tolerance Test
| 2-Hour Plasma Glucose Result (mg/dL) |
Diagnosis |
139 and below |
Normal |
140 to 199 |
Pre-diabetes
(impaired glucose tolerance) |
200 and above |
Diabetes* |
*Confirmed by repeating the test on a different day.
Gestational diabetes is also diagnosed based on plasma glucose values measured during the OGTT. Blood glucose levels are checked four times during the test. If that persons blood glucose levels are above normal at least twice during the test, she have gestational diabetes. Table 3 shows the above-normal results for the OGTT for gestational diabetes.
Table 3. Gestational Diabetes: Above-Normal
Results for the Oral Glucose Tolerance Test
|
Plasma Glucose Result (mg/dL) |
Fasting |
95 or higher |
At 1 hour |
180 or higher |
At 2 hours |
155 or higher |
At 3 hours |
140 or higher |
Urine glucose measurement, once commonly used, is no longer used for diagnosis or monitoring because it is neither sensitive nor specific.
4. DIABETIC RETINOPATHY
Top
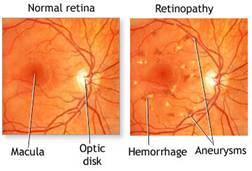
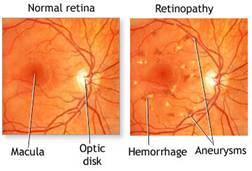
Prolonged high blood sugar in a diabetic patient produces changes in the blood vessels all over the body. The damage to the blood vessels of the retina is called Diabetic Retinopathy. The blood vessels in the retina can be examined directly and non invasively and so even the earliest changes can be diagnosed.
Highlights of Diabetic Retinopathy
-
Diabetic retinopathy can be assessed only by retinal examination.
-
Retinal test is different from glasses testing.
-
Beware! Early stages of diabetic retinopathy will not produce any sight loss.
-
Hence only by retinal examination diabetic retinopathy can be diagnosed.
-
Retinal examination should be done once a year.
Types of Diabetic Retinopathy
Non-Proliferative Diabetic Retinopathy (NPDR)
Proliferative Diabetic Retinopathy (PDR)
In early diabetic retinopathy there are small dilations of the capillary walls in the retina which is called as micro aneurysms. At this stage good control of diabetes and regular follow up examination of the retina is necessary.
In the next stage, small haemorrhages, accumulation of fluid, cells and fat can occur. This is the warning stage and there is no specific treatment even in this stage. The point to be noted here is that sight will not decrease in these stages and so retinopathy can be detected only by routine examination.
In severe cases fluid can collect in the critical “seeing area” of the retina called Macula. Mild to moderate disturbances in the vision may be present. Laser photocoagulation can be done to bring down the fluid accumulation and prevent permanent damage to macula.
In proliferative diabetic retinopathy, abnormal blood vessels develop in the retina, which are very weak and have a tendency to bleed. Once there is a bleed there will be sudden and sometimes total loss of sight. Once there is sight threatening retinopathy, a test called Fundus Fluorescein Angiography (FFA) and laser treatment should be done.
For diabetic patients the level for LDL (bad) cholesterol should be less than 100 mg/dl. Triglycerides in the blood tend to be high when blood glucose is high. High triglycerides also tend to lower the HDL or the good cholesterol.
5. DIABETES AND KIDNEY
Top
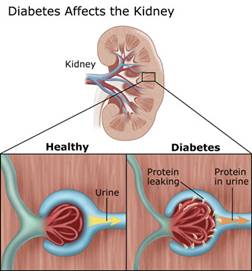
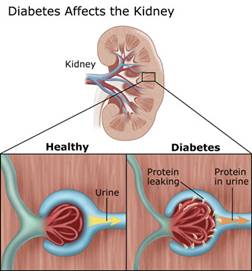
Diabetes is one of the most common systemic diseases to affect the KIDNEY
Kidney damage
Small blood vessels in the kidney filter out the waste products from the body. High blood pressure and high blood sugar can damage these vessels thereby they will not be able to do their functions effectively.
Stages of diabetic kidney damage
In the beginning stages of kidney damage, traces of protein also called 'albumin' begins to appear in the urine. This stage is called MICROALBUMINURIA. Early kidney damage has no symptoms and can be treated with diet and medicines and is reversible.
As the kidney damage gets worse, large amounts of protein can be detected in the urine which is called as the stage of PROTEINURIA or overt nephropathy. By this stage, the damage is often irreversible in most cases. Finally the stage of renal failure sets which can rapidly progress to End stage Renal Disease which requires either Dialysis or Transplantation to sustain life.
INVESTIGATIONS
If albuminuria is detected the following investigations are recommended :-
-
Check for the history of other renal diseases in the family.
-
Check for urinary tract infection through urine and culture sensitivity test.
-
Ultrasound examination of the kidneys.
-
Measurement of urea and serum creatinine and comparison with previous levels.
-
24 hr urine collection for protein excretion.
-
Blood pressure measurement.
-
Check ECG and Chest X-ray.
-
Retinal examination.
RISK FACTORS LEADING TO KIDNEY DISEASE
1. Poor control of diabetes.
2. Long duration of diabetes.
3. Uncontrolled blood pressure.
4. Genetic Factors (Family History of kidney disease).
Prevention of kidney disease
1. Diagnosing diabetes at an early stage by regular screening.
2. Once diabetes is diagnosed, it should be kept under very good control.
3. Tight control of blood pressure (130/80mm/Hg) helps to prevent kidney damage.
4. Regular screening for microalbuminuria to identify early stages of kidney damage.
5. Use of ACE inhibitors or other drugs, which have very good effect in early stages of kidney disease.
6. Regular check up at diabetes centre.
7. Strict diet as advised. If there is proteinuria, the protein intake in the diet may have to be reduced.
Note
* Diabetic kidney disease is one of the commonest causes of kidney failure.
* Kidney disease is asymptomatic till late stages.
* Kidney disease is preventable by early detection of diabetes and good control of diabetes and blood pressure.
* Screening for diabetic kidney disease should be done at least annually.
6. DIABETES AND FEET
Top
As diabetic patients age or the duration of diabetes increases, they may develop diminished sensation and decreased peripheral circulation in the feet and thus are at an increased risk of developing foot infections, especially in those will poorly regulated diabetes.

COMMON PROBLEMS IN DIABETIC FOOT
1. Decreased Blood Supply (Ischaemia)
The ischaemic leg, besides absent or reduced pulses, also has other characteristic features. The skin may become thin and there is usually loss of hair on the foot and ankle. Fissures are very common and ulcers may be painful. It may also be cold to touch.
2. Decreased Sensation (Neuropathy)
The neuropathic foot also has some characteristic features. The feet tend to be warm and dry and relatively insensitive to touch. Neuropathy may affect the muscles of the foot causing clawing of the foot. All this causes the fat pads covering the bones of the feet to be moved away from its position, thus exposing it to weight bearing areas. Any weight bearing area without adequate protection tends to open and form a wound called as an ulcer.
In order to protect the leg, nature offers a mechanism by which it thickens the skin to avoid forming a wound. This protective mechanism will lead to problems such as callus and corns in later stages due to irritation of the tissues beneath. These can break down and lead to ulcers.
3. Infection
Both ischaemic and neuropathic lesions are commonly complicated by infection. Common symptoms of infection are fever, redness, swelling or pain. Pus may also be seen in the lesions.
4. Combined Lesions
It is common for a patient to have all the processes mentioned above occurring at the same time. Thus a person can have an infected, neuropathic lesion with poor blood circulation.
7. PREVENTION OF DIABETES
Top
The prevalence of Diabetes Mellitus in the Indian population now ranks first in the world even ahead of China. In the last twenty years there has been a three fold increase in the prevalence of diabetes and today it is estimated that there are over 32 million people with diabetes in India.
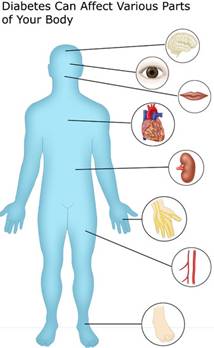
The problem in diabetes is that very often it is silent. The symptoms of diabetes such as increased thirst and urination, etc., occur only when the diabetes is severe. In early stages it can remain totally asymptomatic. Moreover after 10-15 years duration of diabetes, the prevalence of all diabetes related complications increase markedly. These include Retinopathy leading to blindness, Nephropathy leading to kidney failure, Heart attacks, Gangrene of the feet, Stroke and even less known complications like Impotency, or sexual weakness. Thus diabetes is a serious threat to public health and this shows the urgent need for prevention of diabetes.

I. PRIMARY PREVENTION
Primary prevention refers to the prevention or the postponement of diabetes in those who are susceptible to diabetes. Early detection is the key to prevent and control diabetes. As diabetes is largely asymptomatic, regular screening for diabetes is most important.
Indications for screening:
1. Positive Family History
It is a well known fact that diabetes is caused mostly due to hereditary factors. Hence it is clear that screening of diabetic families would be the first priority.
Risk of diabetes based
If both parents are diabetic 99%
If one parent is diabetic 50%
If any other relative is diabetic 25%
Hence it is clear that any one who has positive family history should be screened for diabetes.
Screening
The onset of diabetes is earlier in Indians i.e., around 20-30 years of age. If the family history is strong, e.g., members of more than two generation in the family have diabetes, the first screening could be done even by 20 years of age and thereafter on a yearly or two yearly basis.
2. Obesity
Obesity causes resistance to Insulin. Your body makes insulin but the extra weight prevents it from using the insulin the way it should be used. For this reason, obesity is another risk factor for diabetes.
3. Physical inactivity (those with sedentary jobs)
The Glucose Tolerance Test (GTT) is the confirmatory test since it helps to diagnose even the early stage of diabetes. Most people check only Fasting, Postprandial or Random Blood Sugar which may not reveal diabetes until it is at a more advanced stage. Even if the GTT results show normal values at the time of testing, it does not mean that the person will never develop diabetes. Such individuals should have an annual GTT done if the family history of diabetes is very strong.
II. SECONDARY PREVENTION
Secondary Prevention refers to the prevention of complications once diabetes set in. This can be achieved by good control of diabetes with the help of diet, exercise, medication and regular monitoring of blood sugars. Blood sugars can be checked even on daily basis with the help of blood sugar meters which facilitates quick determination of blood sugars. Since blood sugars tend to fluctuate a lot, from day to day or hour to hour, HbA1C (Glycosylated haemoglobin) test should be done to assess the blood sugar for the previous 2-3 months.
III. TERTIARY PREVENTION
Tertiary prevention refers to the rehabilitative measures once the complications have set in. For example, for Diabetic Retinopathy, Laser Photocoagulation will help to prevent or reduce the incidence of blindness. Laser photocoagulation helps to seal leaking blood vessels in the retina and thus prevent visual loss.
It is recommended that at least once a year every diabetic individual should do a complete check-up of all complications especially the eyes, kidneys, heart and feet in order to reduce the morbidity due to diabetes.
EXERCISE & DIABETES
1. Reduces weight
2. Improves blood sugar control
3. Reduces the dose of diabetic medications
4. Improves the quality of life
Tips for smart and safe exercise
1. Consult your doctor before beginning exercise programme.
2. Always carry a diabetic identity card.
3. Stay alert for signs of low blood sugar during or several hours after exercise.
4. Have rapidly absorbable carbohydrate sources ready like sugar, glucose and candy.
5. Monitor blood sugars before and after the exercise.
6. Take carbohydrate snacks if blood glucose levels are less than 100 mg/dl.
7. Drink plenty of fluids before and after and if necessary during exercise to avoid dehydration.
Time: Exercise should last for at least 30 minutes and go up to one hour if possible. There should be a warm up and cool down period for each session.
Warm up - Prepares body for vigorous activity; helps prevent strains and injuries to muscles. It should last for 5-10 minutes.
Cool down - Helps restore circulation to normal levels, prevents cramps, sore muscles and post-exercise dizziness. This should also last for 5 - 10 minutes.
8. DIET AND DIABETES
Top
Objectives
-
To maintain adequate nutrition
-
To achieve and maintain desirable body weight
-
To maintain normal blood sugar levels
-
To prevent, delay or minimize the onset of chronic degenerative complications
Diet plays an important role in the treatment of diabetes. The diet may be used alone or in combination with insulin injections or oral hypoglycaemic drugs.
The diet plan of an individual is based on height, weight, age, sex, physical activity and nature of diabetes.
Tne should consider the following points while planning a diabetic diet:
-
Determining energy requirements
-
Determining the type of carbohydrates, fibre and food preparations
-
Presence of any other complication such as high blood pressure, high cholesterol levels etc.
Diet is the most important aspect in the treatment of diabetes, but there is no single diabetes diet. The old idea that Rice should not be taken is a fallacy. All cereals contain the same amount of starch. e.g., rice, wheat, jowar etc. It is the quantity that matters.
Vegetable proteins like dhal, pulses and legumes are better than animal proteins. Combination of cereals and pulses will enhance the protein quality. Mushrooms are low in calorie, but rich in protein.
Fibre rich foods are very good in controlling diabetes and for reducing serum cholesterol. Rich sources of natural fibre are whole cereals, pulses like bengal gram, black gram, green gram and green leafy vegetables. Soluble fibres from fenugreek seeds taken either as sprouted or in powder form can be used as a supportive therapy.
Intake of saturated fat should be reduced to prevent increase in serum cholesterol. Use vegetable oils in moderation and a mixture of monounsaturated oils like groundnut or gingelly oil and polyunsaturated oils like saffola or Sunola is best.
The intake of total calories is to be reduced by those who are overweight.
Food should be distributed into small frequent feeds. Skipping a meal or fasting is not really advisable.
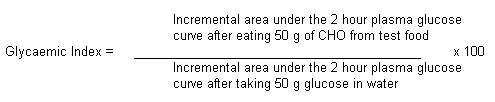
GLYCAEMIC INDEX
The rise of blood sugar after a meal does not merely depend upon the amount of carbohydrate ingested but also the rapidity of absorption which varies with the fibre content, phytate, tannins and enzyme inhibitors.
The ability of the food item to raise the blood sugar is measured in terms of glycaemic index.
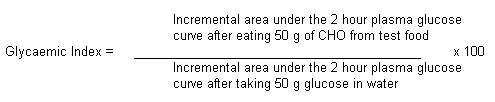
Diabetics prefer low glycaemic foods
Factors affecting the glycaemic response to food
-
Rate of ingestion
-
Food form
-
Food components
- Fat content
- Fibre content
- Protein content
- Starch characteristics
- Food ingredients
4. Methods of cooking and processing food
5. Physiologic effects
6.Colonic effects
Rate of ingestion: Sipping 50g of glucose slowly over a several hour period produces a much smaller increase in blood glucose than rapid intake of the same amount.
Food form: Consumption of ground rice raises the blood sugar level to a greater extent than of unground rice.
Food components: Fat, fibre, protein and type of starches influence glycaemic index as they affect the rapidity of absorption.
Foods rich in fat and protein like ice creams, groundnut and milk have low glycaemic index. But they are not recommended for diabetics because they have high calorific value. Pulses which have high protein are low in glycaemic index compared to cereals.
Foods with soluble fibre such as beans, have a low glycaemic index. Some starches are more slowly digested either because they are protected in structure or because the molecule is unbranched (amylose). Phytic acid, usually contained in cereals and pulses may have a more dominant role in decreasing the blood sugar rise than fibre.
Fructose produces lower rise of blood sugar than glucose. In view of its effect on serum lipid, it is not preferred.
Method of cooking and processing: Chapathis which need chewing have lower glycaemic index compared to 'wheat kanjee'.
Glycaemic response is higher with cooked than raw food.
Physiological effects: Digestion of dietary carbohydrate in the upper gastrointestinal tract provides glucose, fructose and galactose for intestinal absorption. The presence of non-absorbable oligosaccharides and viscous dietary fibres such as pectins, B-glucous and gums in fruits, vegetables and cereals reduces the efficiency of enzyme hydrolysis and slows the rate at which glucose enters the blood stream.
Starch encased in its seed coat or coarsely ground is not efficiently hydrolysed to glucose because digestive enzymes are prevented from reaching the starch. Starch granules subjected to moist heat and subsequent cooling become dense and less available to enzyme action. Thus the physical form as well as food processing and cooking methods influence the energy availability of dietary carbohydrate.
High glycaemic foods (65-75%) -Wheat, rice, root vegetables
Intermediate glycaemic foods (45-55%) - Fruits
Low glycaemic foods (30-40%) - Legumes.
Glycaemic index of common foods
| Item |
Glycaemic Index |
Cereal Products |
Bread |
70 |
Millets |
71 |
Rice (White) |
72 |
Wheat (Paratha) |
70 |
Breakfast Snacks |
Pongal |
55 |
Pesarattu |
60 |
Upma |
75 |
Idli |
80 |
Chole |
65 |
Sprouted green |
Gram |
60 |
Sundal |
80 |
Dairy products |
Milk |
33 |
Ice-cream |
36 |
Curds |
36 |
Miscellaneous |
Groundnuts |
13 |
Potato chips |
51 |
Tomato soup |
38 |
Fruits |
Apple |
39 |
Banana |
69 |
Orange |
40 |
Vegetables |
Brown beans |
79 |
Frozen beans |
51 |
Potato |
70 |
Sweet potato |
48 |
Yam |
51 |
Beetroot |
64 |
Dried Legumes |
Soya beans |
43 |
Rajmah |
29 |
Bengal gram |
47 |
Green gram |
48 |
Black gram |
48 |
Sugars |
Fructose |
20 |
Glucose |
100 |
Maltose |
105 |
Sucrose |
59 |
Honey |
87 |
-
High glycaemic foods (65-75%)-wheat, rice, root vegetables
-
Intermediate glycaemic foods (45-55%)-Fruits
-
Low glycaemic foods (30-40%)-Legumes
In general, high-fibre foods with low glycaemic indices (e.g., beans, vegetables, whole fruit and whole grains) are the preferred forms of carbohydrate in a defensive nutrition plan. Meal combination is also an important factor in managing blood glucose levels. Combining protein, fat and carbohydrate at meals and snacks i.e., small serving of nuts and a piece of fruit, can lead to better control of blood glucose levels and less insulin release than meals or snacks that consist mainly of carbohydrate like bread and jam.
Soluble dietary fibre combined with lower glycaemic index food is good for diabetics.
FOODS TO BE INCLUDED
Skimmed buttermilk, unsweetened lime/tomato juice, clear soup, pepper water (rasam), vegetable salads like tomatoes, cucumber, onion, white radish, lettuce and capsicum. Vegetables that can be taken in unlimited amounts are - Ash gourd, Beans, Bitter gourd, Bottle gourd, Brinjal, Brussels sprouts, Broccoli, Cabbage, Cucumber, Cauliflower, Chow-chow, Cluster beans, Coriander leaves, Cowpea-pod (Karamani), Capsicum, Drumstick, Ginger , Greens (all varieties), Knol khol, Kovai, Ladies finger, Mint, Onions, Papaya (raw), Plantain flower, Plantain stem, Ridge gourd, Snake gourd, Tomato (raw and ripe), Turnip, White Radish.
Carrot, beetroot, peas and double beans can be used in moderation
FOODS TO BE AVOIDED
Sugar, honey, glucose, jam, jaggery, sweets, cakes, pastries, tender coconut water sweetened, soft drinks, banana, mango, jack fruit, potatoes, yam, colocasia and tapioca, custard apple (Sitaphal) and dry fruits, especially if overweight.
Apple, orange, sweet lime, papaya, guava, pear, muskmelon and watermelon etc., may be taken in consultation with Diabetologist /Dietitian when blood sugar is under control.
Food items that are equivalent to 200 calories are:-
3 Idlies (or) 3 Chappaties (or) 2 Dosas (or) 1-3/4 cups of Rice. (Remember: any one and not all of these)
| Food groups |
High fibre foods |
Low fibre foods |
Cereals |
Whole cereals like whole wheat, dalia, whole wheat flour |
Refined cereals like rice, bread, maida, suji, noodles, macaroni, etc |
Milk and milk products |
- |
Milk and milk products |
Pulses |
Whole dhals and dhals with husk |
Washed dhals |
Meat, fish and poultry |
- |
Eggs, chicken, fish |
Vegetables |
Vegetables like peas, beans, lotus stem etc. |
Vegetables like potato. |
Fruits |
Fruits like apple, cherries, pears, peaches, plums, guava etc. |
Fruit juices and fruits like banana and papaya |
Fats |
- |
Fats |
To remember
-
It is important to control the amount and time of food intake.
-
Meals should not be missed.
-
Consider the likes and dislikes of the patient.
-
Try to substitute the craving for sweet by taking some fruit.
Source
Jenkins et aI., 1981; Am. J. Clin. Nutr., 34: 392, 1981.
Raghuram et aI., Diabetes Bull., 7: 64, 1987.
Dilwari et al., Diet, Digestion & Diabetes, 1987.
Cited from: Raghuram, T. C. et al, 2000, Diet and Diabetes, National Institute of Nutrition, Hyderabad, 500 007.
Srilakshmi .B 2003.Dietetics, New Age International (P) Publishers Ltd.Chennai.
http://doctor.ndtv.com/Diabetes/
http://www.health-and-holistic-wellness.com/image-files/diabetes1.jpg
http://www.health-and-holistic-wellness.com/image-files/diabetes2.jpg
http://www.deo.ucsf.edu/images/charts/5.a.jpg
http://ucsf.mightyminnow.com/images/charts/5.c.jpg
http://assets.aarp.org/external_sites/adam/graphics/images/en/19290.jpg
http://www.railwayhospital.com/stories/diabetes/diabetic-retinopathy.jpg
http://media.photobucket.com/image/raw%20vegetable%20salad/IMG_1733.jpg
http://www.gotethnicfoods.com/pictures/Regular/DFK45.jpg
http://www.onlinegardenertips.com/images/What-Is-Potato-Plant-Pesticide.jpg
http://www.dkimages.com/discover/previews/1101/10446126.JPG
http://cookingwithkimberly.com/wp-content/uploads/2008/01/orangejuice.jpg |